
Ankle Fusion
Ankle Fusion
Ankle Fusion (Arthrodesis)
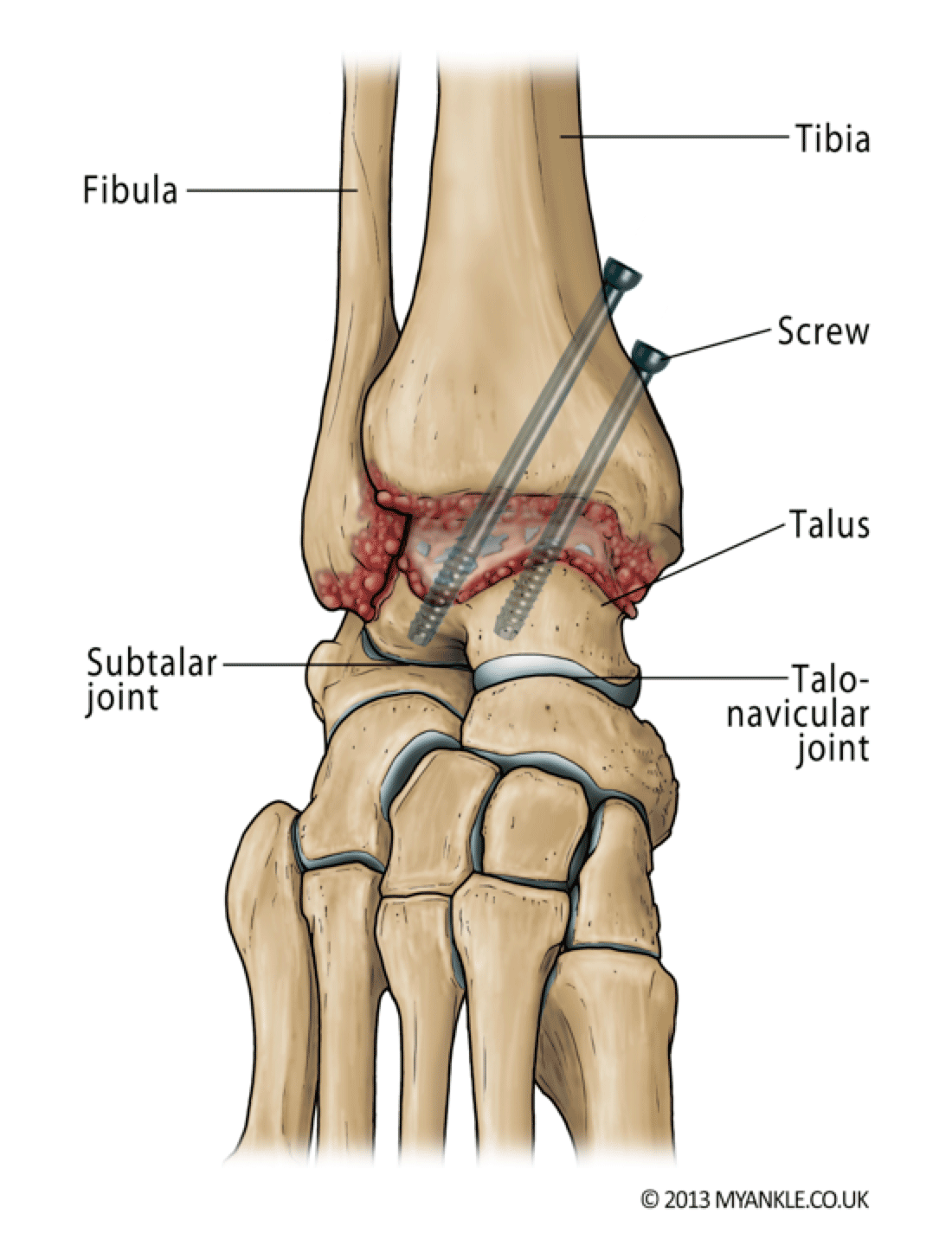
Ankle fusion is an operation to convert a stiff painful joint into an even stiffer but painless joint. In this procedure, the remaining damaged cartilage is removed from the ends of the bone and the two bones are then held together in compression using screws, or plates until they join to become one (bone fusion).
Ankle fusion affords excellent-pain relief and good function.
A variety of techniques are available to achieve a stable fusion, including arthroscopic (keyhole surgery) and open surgery. The most common technique in the UK is arthroscopic ankle fusion where the joint surfaces are prepared through a telescope and two or three screws are inserted through small incisions, going across the joint to hold the two ends together.
In complex deformity or where the subtalar joint (the joint below the ankle) is also affected, a tibiotalocalcaneal (TTC) intramedullary nail might be necessary.
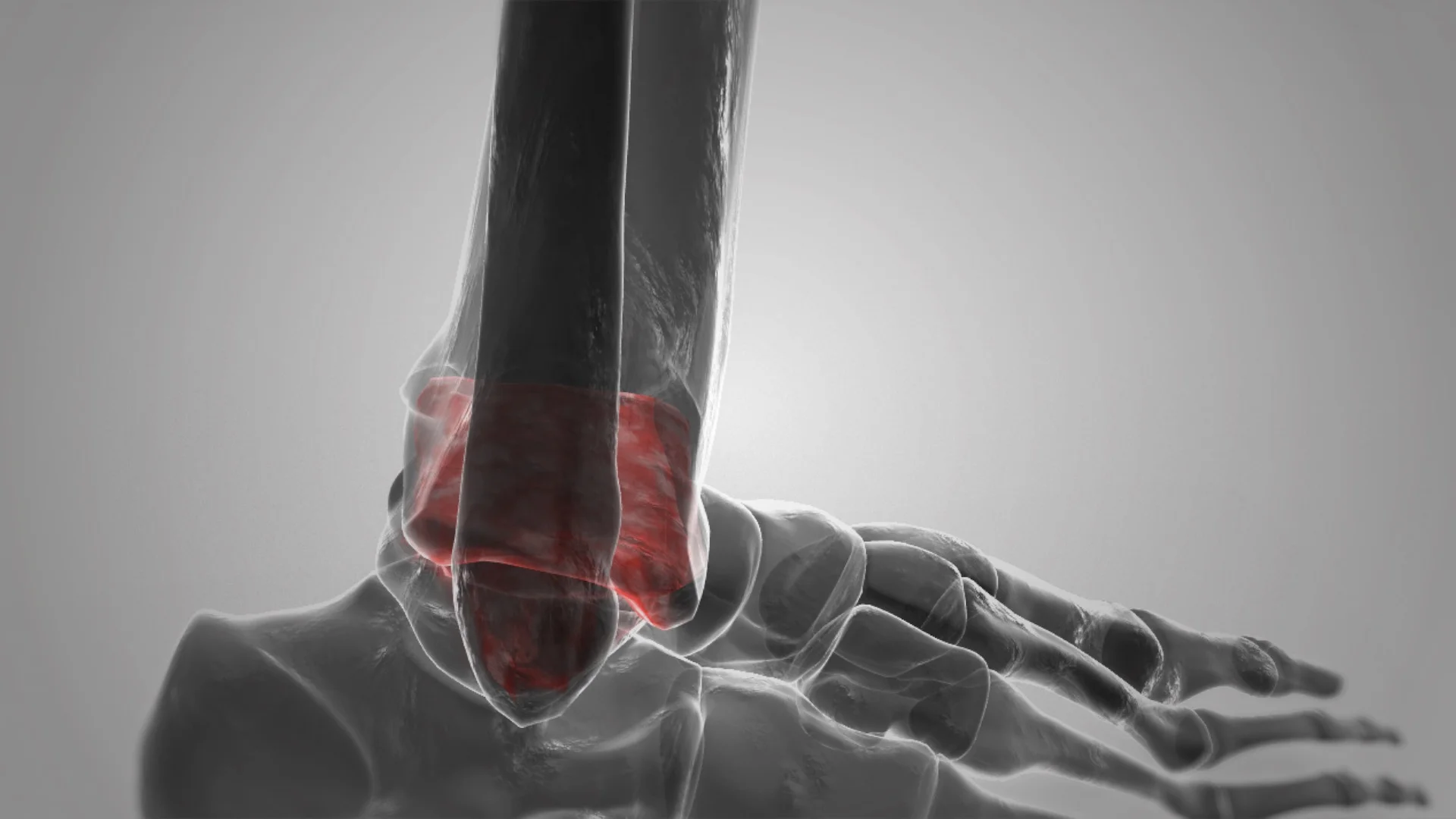
Ankle fusion does have its limitations including prolonged immobilization and the risk of non-union (the bones not knitting). Because the ankle joint has been stiffened, more stresses will be taken by adjacent joints which are at risk of wearing with time (adjacent-joint arthritis). X-ray features of adjacent joint arthritis are common after 10 years, but not all patients will require treatment for this.
Biomechanical studies have shown that ankle fusion increases contact stress at the talonavicular and calcaneocuboid Joint. At 44 months follow-up, following ankle fusion, patients demonstrated reduced cadence and stride length accompanied by a diminished range of motion of the hindfoot and midfoot during walking.
In a study of 28 patients who all stated they were highly satisfied immediately after ankle fusion, 79% reported difficulty walking on uneven ground, and 64% reported aching around the ankle with prolonged standing or walking.
Post Op
This video shows a man 1 year post arthroscopic ankle fusion. He is able to stand on his tiptoes and jog, albeit with a slight limp.
Are there many major risks with ankle fusion?
In addition to the general risks of ankle surgery, the specific risks of ankle arthrodesis relate to problems with union and transference of stress to the adjacent joints.
Mal-Union: Research has shown that 5 to 10% of fusions do not heal in the exact position intended. This may either be due to the fact that the position was not achieved at the time of surgery or that the bones have shifted while in plaster. This does not usually cause any major problems but rarely further surgery may be required to correct this.
Adjacent Joint Arthritis: Because the ankle joint has been stiffened, more pressure will be taken by adjacent joints, which, with time, are at risk of wearing . Signs of arthritis in the adjacent joints are common on x-rays after 10 years, but many patients do not require treatment for this.
Need for Further Surgery: Sometimes the screws become prominent under the skin. If this happens, they can be removed but only about 1 in 10 patients need the screws to be taken out. If screws need removing, we usually advise you to wait at least a year after surgery to give the bones time to become strong.
General complications following ankle surgery:
Swelling – you should expect some swelling for up to one year after surgery. Elevation of limb above heart level for the first two weeks helps to reduce swelling and aid wound healing. If swelling persists and you are concerned, seek medical advice.
Bleeding – all wounds bleed after surgery, but rarely this can be excessive causing wound problems or requiring further surgery.
Painful scar – any type of surgery will leave a scar. Some people develop larger scars than others. Occasionally this can cause pain and irritation. If you suspect you are prone to scar problems please discuss this with your surgeon prior to surgery.
Infection – superficial wound infection (redness around the wound) occurs in up to 5% of cases. Much rarer (less than 1%) is a deep infection where the metalwork or bone is infected. Minor infections usually clear up with a course of antibiotics. More serious infections may require further surgery and involve complex and lengthy treatment.
Nerve injury – numbness or tingling at the surgical site is common and is usually temporary, but up to 50% of patients who have an ankle replacement or open ankle fusion will get some numbness on the top of their foot. This is not usually a problem. If a key nerve is injured (up to 1.5% of cases) then it can cause permanent numbness and shooting pains requiring medication or further specialist input. Rarely the sympathetic nerves (also known as fight or flight nerves) react badly after the surgery, and cause temperature and colour changes to the skin – this is known as complex regional pain syndrome (less than 3%) and can take up to 12-18 months to settle. Occasionally it does not settle and causes long term pain.
Problems with union – occasionally in arthrodesis bones fail to unite (fuse) and in the case of a replacement, the bones may not knit to the implant. This can happen in up to 10% of patients. If you smoke, your risk of such a complication is greatly increased. You will be advised to stop smoking before surgery.
Blood clots – deep vein thrombosis (DVT) is uncommon (5%), and pulmonary embolus (PE) is very rare (less than 0.5%) and occurs due to blood clots. We do everything to minimise these risks but they can occur and can be serious causing prolonged leg swelling or chest problems. Blood-thinning medication may be given to prevent blood clots whilst in a cast as well as a special stocking on the other leg to improve venous circulation.
Ankle fusion is the most commonly performed surgical treatment of end stage ankle osteoarthritis but does carry the risk of adjacent joint arthritis. Patients should be counselled regarding the benefits and risks of both ankle fusion and replacement as well as the potential for non operative treatments.
Ankle Replacement
Ankle Replacement
Ankle Replacement
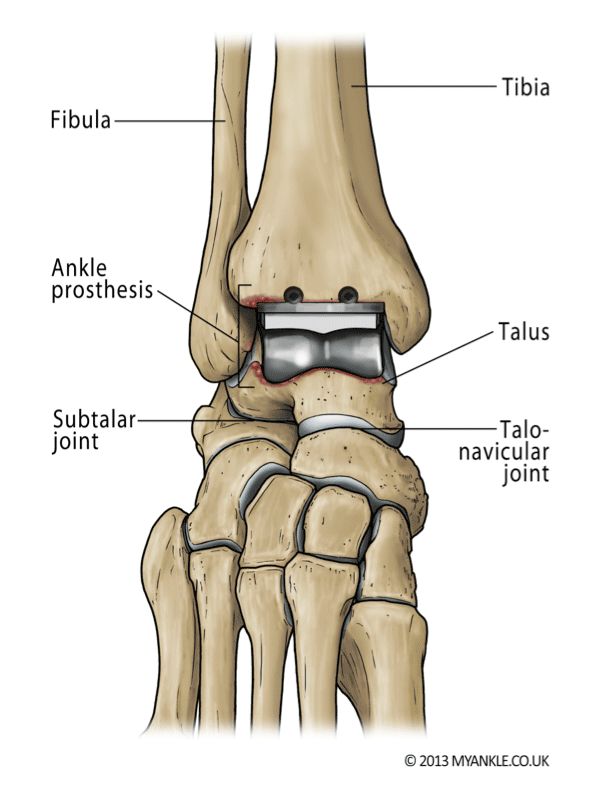
Total ankle replacement is an operation to replace a worn-out ankle joint by resurfacing the ends of your tibia and talus with metal components with a plastic insert in between them to allow gliding motion.
The metal components are fixed into bones using pegs or stems and have a special coating to encourage the patient’s bone to grow into them. Total ankle replacement (TAR) is an emerging technology. Although the first generation of total ankle replacements in the 1970’s showed poor results, improvements in technology and research have led to the development of a third generation of uncemented, three component, mobile-bearing implants.
In the UK, most ankle replacements have a mobile component, made of ultrahigh molecular weight polyethylene (hard wearing plastic), which sits freely between the talar and tibial components and moves forwards and backwards slightly during ankle motion. In some ankle replacements the plastic is fixed to the tibial component, and this is known as a two-component or fixed bearing ankle replacement. No one knows whether a fixed bearing or mobile bearing implant is better, and the choice of implant should be discussed with your surgeon.
There are now more than 11 different prostheses on the market in the UK although at present there is no clear advantage of one prosthesis over another and we recommend that you discuss the type of prosthesis with your surgeon.
There are recognised contraindications to ankle replacement and these include, severe osteoporosis, severe avascular necrosis, uncontrolled diabetes, ligament instability and significant deformity.
An ankle replacement is performed through an incision over the front of the ankle. The surgery takes between one and two hours and you will have a tourniquet applied around your thigh during the surgery, to reduce bleeding.
When you wake from surgery you will have a below knee partial cast, which may later be changed into a full below knee plaster or synthetic cast. You may have to wear a cast for a period of up to 6 weeks. In some circumstances your surgeon may choose not to use a cast but may use a walker boot instead.
You are likely to need crutches or a frame to help you walk. Depending on your situation, your surgeon may allow you to fully weight bear immediately in the cast or walker boot.
One of the main reasons for a cast after this surgery relates to the healing of the wound. The blood supply to the skin at the front of the ankle is poor and motion of the tendons under the skin sometimes slows healing. Where your skin condition is a concern or if you have had more complicated surgery, you may be advised to non-weight bear for up to 6 weeks.
Because of the immobility it is usually recommended that you have blood-thinning medication to prevent blood clots whilst in a cast as well as a special stocking on the other leg to improve blood flow.
After your boot or cast is removed you should be able to wear normal shoes. In some cases you may require an ankle brace or a walking boot for a short period as guided by your surgeon.
What can I expect after an ankle replacement
Total ankle replacement provides excellent-pain relief and good function, and has a greater than 90% success rate, as measured by patient satisfaction in the short term, but like all joint replacements is prone to wear and failure with time. This appears more likely to occur in ankle replacement than in hip or knee replacements.
In most cases the range of motion after a replacement is better than before, but in some patients this is not the case, largely due to stiffness and scarring of the soft tissues. It is important that you discuss the likely range of movement you should expect with your surgeon before having your surgery, as this helps you to have realistic expectations.
Walking: In most cases, walking will be normal, so that others may not notice that you have had an ankle replacement. If you walked with a limp prior to surgery because of pain, after the surgery your walking is likely to improve.
Sports: You should be able to return to long walks, hiking, cycling and certain sports such as golf, although it might take up to 18 months before you find it comfortable to do.
Although there are cases where patients have returned to more vigorous activities such as squash, tennis or jogging, we do not recommend them, as they put a lot of stress on the replaced joint which is likely to wear and fail more quickly. There is also a risk of putting stress across the adjacent joints which might wear even in the presence of an ankle replacement.
Post Op
This video shows a 70 year old male, 6 months following an ankle replacement. He had quite significant hind foot deformity prior to the ankle replacement and so also underwent a cavo-varus foot correction with a heel shift and dorsiflexion osteotomy of his big toe. He is able to walk and tip toe without noticeable difference to the unaffected side.
This video shows a lady that has undergone an ankle replacement 6 months earlier. She is able to tip toe and walk without a discernible limp.
Are there any major risks with an ankle replacement?
In addition to the general risks of ankle surgery, the main risks of ankle replacements are due to them being a new technology with uncertain long-term results.
Need for Revision: Research suggests that ankle replacements are not yet as reliable as hip or knee replacements. Approximately 80-90% of ankle replacements will still be in place 10 years after surgery, while some ankle replacements will loosen early (within 1-2 years) and require surgery sooner rather than later. The commonest reason for an ankle replacement to fail is loosening of the metal components. This might be accompanied by cysts that have formed due to wear of the plastic component. If the ankle does wear out, becomes loose or “fails”, then it can be removed and revised. Revision can either be to another ankle replacement or conversion to an ankle arthrodesis (fusion). An arthrodesis following ankle replacement is usually successful, but is a bigger operation than if it was done in the first place.
Ongoing Pain: In up to 10% of patients with ankle replacement, there remains some pain in the ankle, which is not easily explainable, as the X-rays look fine. Although in most cases these symptoms disappear after 12-18 months, a small proportion continue to have pain and require either a reoperation or revision surgery.
General complications following any ankle surgery:
Swelling – you should expect some swelling for up to one year after surgery. Elevation of limb above heart level for the first two weeks helps to reduce swelling and aid wound healing. If swelling persists and you are concerned, seek medical advice.
Bleeding – all wounds bleed after surgery, but rarely this can be excessive causing wound problems or requiring further surgery.
Painful scar – any type of surgery will leave a scar. Some people develop larger scars than others. Occasionally this can cause pain and irritation. If you suspect you are prone to scar problems please discuss this with your surgeon prior to surgery.
Infection - superficial wound infection (redness around the wound) occurs in up to 5% of cases. Much rarer (less than 1%) is a deep infection where the metalwork or bone is infected. Minor infections usually clear up with a course of antibiotics. More serious infections may require further surgery and involve complex and lengthy treatment.
Nerve injury – numbness or tingling at the surgical site is common and is usually temporary, but up to 50% of patients who have an ankle replacement or open ankle fusion will get some numbness on the top of their foot. This is not usually a problem. If a key nerve is injured (up to 1.5% of cases) then it can cause permanent numbness and shooting pains requiring medication or further specialist input. Rarely the sympathetic nerves (also known as fight or flight nerves) react badly after the surgery, and cause temperature and colour changes to the skin – this is known as complex regional pain syndrome (less than 3%) and can take up to 12-18 months to settle. Occasionally it does not settle and causes long term pain.
Problems with union – occasionally in arthrodesis bones fail to unite (fuse) and in the case of a replacement, the bones may not knit to the implant. This can happen in up to 10% of patients. If you smoke, your risk of such a complication is greatly increased. You will be advised to stop smoking before surgery.
Blood clots – deep vein thrombosis (DVT) is uncommon (5%), and pulmonary embolus (PE) is very rare (less than 0.5%) and occurs due to blood clots. We do everything to minimise these risks but they can occur and can be serious causing prolonged leg swelling or chest problems. Blood-thinning medication may be given to prevent blood clots whilst in a cast as well as a special stocking on the other leg to improve venous circulation.
Audit & Research
There is a mandatory requirement that all ankle replacements implanted in England and Wales should be entered into the UK National Joint Registry. The NJR started to collect total ankle replacement primary and revision procedures on 1st April 2010. More than 2000 TARs have been reported to date. For primary procedures, 56% of the patients were male. The average age of an ankle replacement patient was 66.8 years and had an average BMI of 29.9.