Normal Structure and Function
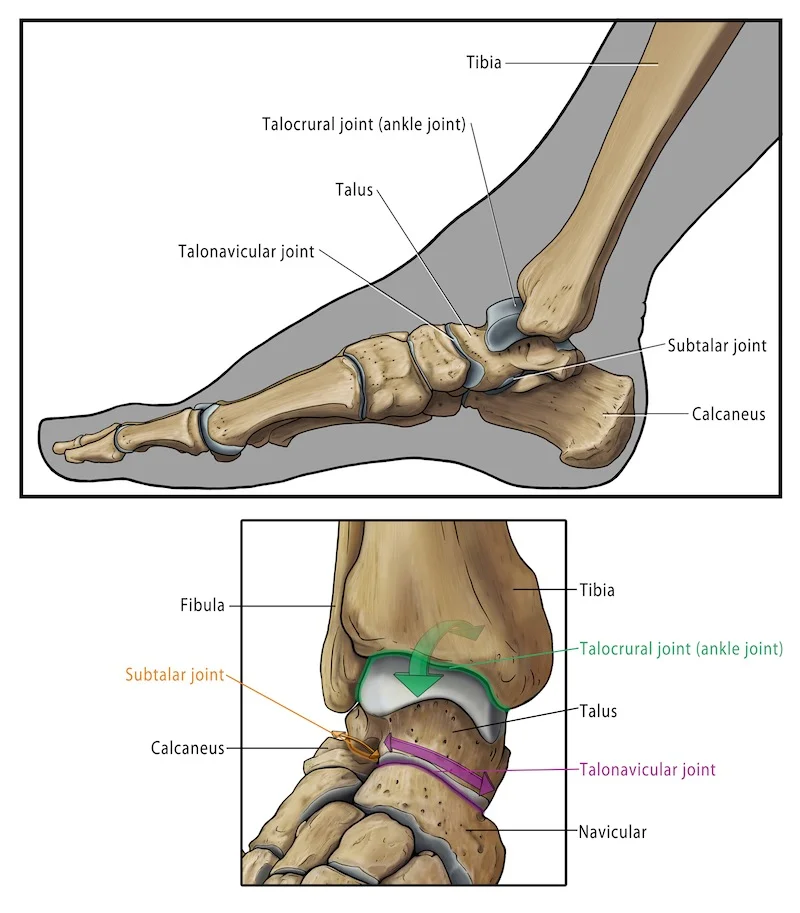
Ankle Arthritis affects the ankle joint, which is formed by the lower end of the tibia (shin bone) and the talus, also known as the tibiotalar joint. The ankle joint works like a hinge allowing upwards and downwards movements, but unlike a hinge, there is also some sliding and rotation of the talus within the ankle joint. In addition, movements also take place in the joints close to the ankle joint. The subtalar joint, or joint below the ankle, is responsible for side-to-side movements, such as walking on an uneven surface. In front of the ankle joint is the talonavicular joint which is involved in the twisting movements of the arch of your foot, which occur when walking. In normal joints there is a layer of cartilage, which acts as a shock absorber and allows smooth gliding motion.
What goes wrong in ankle osteoarthritis?
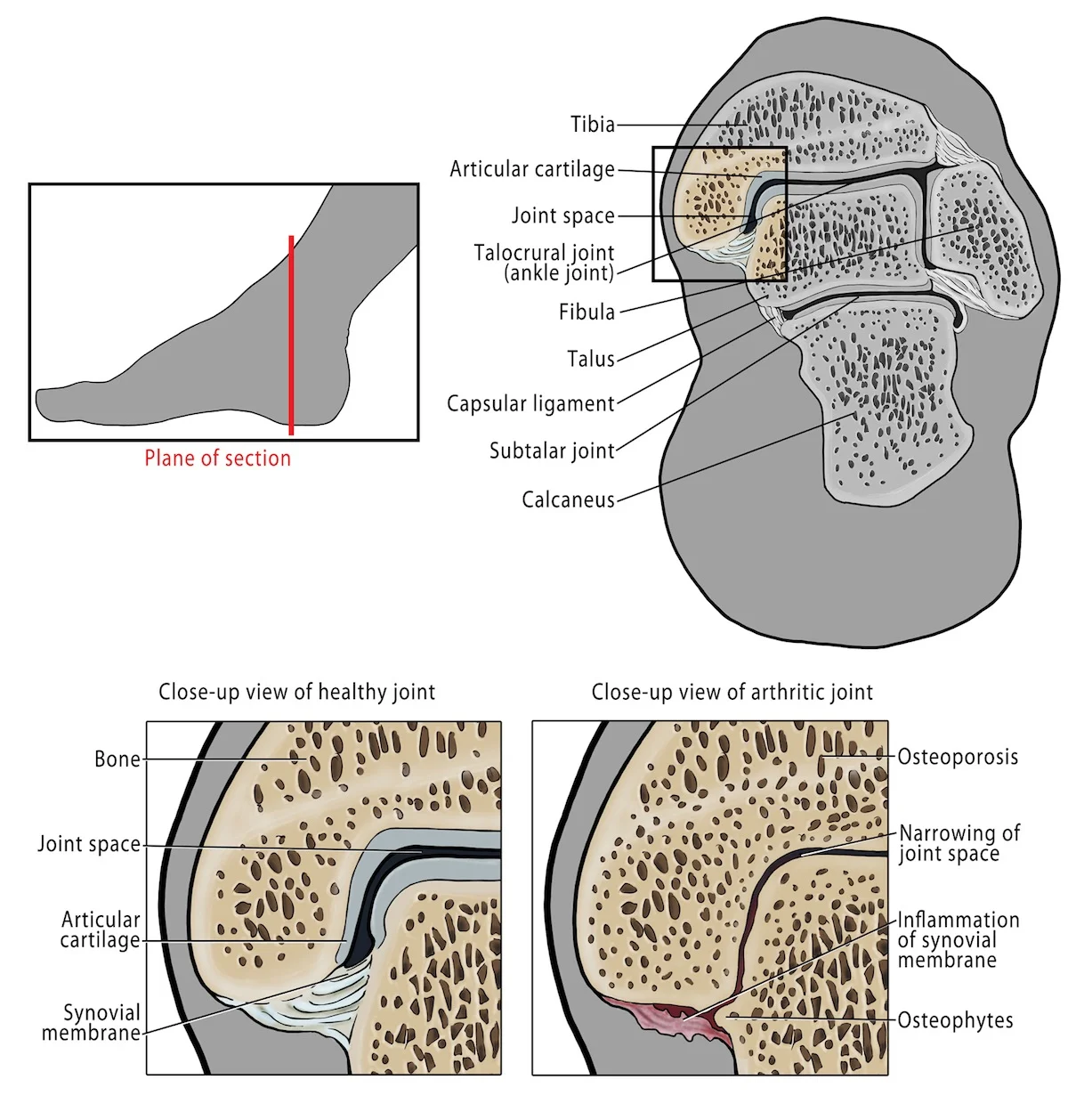
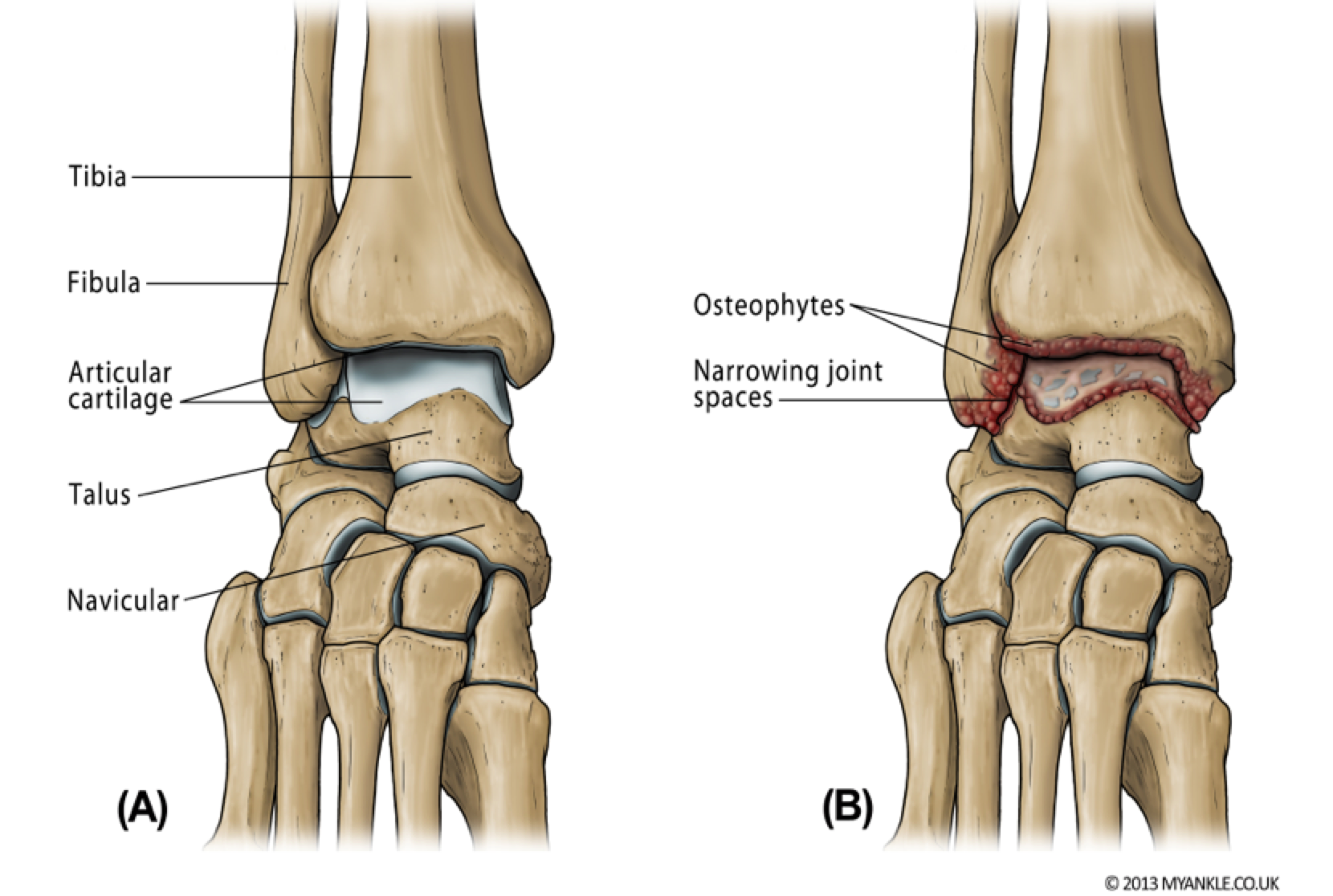
In ankle arthritis the cartilage is worn and the bone starts to rub on the bone, which is painful. As with other joints, the bone surfaces are lined by articular cartilage which is a form of shock absorber allowing smooth gliding motion during walking and running. When this cartilage becomes worn, either as a result of wear and tear or damage following injury or disease, then the normal smooth motion of the joint is affected. Often extra bits of bones form which together with scarring of the joint capsule are responsible for joint stiffness. Ankle arthritis has a similar impact on quality of life as hip arthritis and congestive heart failure.
Ankle osteoarthritis is defined as “end stage”, when all non-surgical treatments have failed.
Causes of osteoarthritis
Ankle arthritis (osteoarthritis) is the end result of the cartilage wearing away. Its causes are primary and secondary.
In primary osteoarthritis there is no known cause and it runs in your genes. You may have swollen painful fingers (Heberden’s and Bouchard’s nodes) and your parents might also have been diagnosed with similar symptoms at a similar age to you.
Osteoarthritis can also be secondary to other injuries or diseases. The commonest cause is post traumatic, that occurs after a severe sprain or fractures around the lower leg. It can also occur secondary to inflammatory arthritis such as rheumatoid arthritis or gout.
The majority of ankle arthritis (OA) follows trauma or injury, although inflammation (such as rheumatoid arthritis) can also be a cause. Over 29,000 cases of symptomatic ankle OA are referred to specialist foot and ankle surgeons each year in the UK. The ankle is injured more than any other joint, indeed ankle sprains are one of the commonest reasons for attending Emergency Departments. The incidence of ankle fractures is increasing especially in young athletes and elderly females. After an unstable ankle fracture, radiographic ankle OA can occur in up to 66% of patients within 6 years. Many patients are afflicted in their sixth decade, during their working life.
Symptoms
Pain
Stiffness
Instability or giving way
Locking
Swelling
Diagnosis
Diagnosis of ankle arthritis is usually made by a specialist orthopaedic foot and ankle surgeon based on taking a history of your problems. They will want to know about any preceding injuries, as well as any past medical and social history and what medication you take. The diagnosis is confirmed by a careful clinical examination and a series of weight bearing X-rays which will usually show a loss of joint space (loss of the lining cartilage), extra bone spurs (osteophytes), bone cysts (fluid that gets into microcracks in the joint surface), and in severe cases, bony deformity.
Investigations
In most cases a standing plain X-ray is all that is needed but your specialist may also want to take some blood tests (usually to look for evidence of inflammatory arthritis such as gout or rheumatoid arthritis). In some situations an MRI scan or CT scan is also necessary.
Non Operative Treatments
Accepted non operative treatments for ankle arthritis include:
Pain Killers
Cutting down on your activity levels
The use of a walking stick
A supportive ankle brace
Physiotherapy
Orthotics and footwear adjustments
Changing your job to a more sedentary one
There are a number of treatments that have no supportive evidence behind them. These include: phonophoresis; prolotherapy; platelet rich plasma (PRP); cryotherapy; viscosupplementation; and acupuncture. None of these have been shown to be effective in treating ankle arthritis and should be avoided as there is no good evidence to support their use, and they should be considered unproven. Nonetheless there are lots of groups offering such treatments citing only anecdotal evidence and we advise you not to be drawn in by someone offering such treatments unless they are part of a registered clinical study.
Intra articular local anaesthetics should only be used for diagnostic purposes by a specialist consultant orthopaedic surgeon.
If non-operative treatments have not worked then you should seek advice of a specialist orthopaedic foot & ankle surgeon to discuss surgery which includes ankle replacement or ankle fusion.